Home

Male Infertility

Azoospermia and Male Fertility: What Every Man Should Know
In this Article
Male Infertility
Azoospermia and Male Fertility: What Every Man Should Know
Updated on 19 June 2023
Sometimes when you feel you have reached a dead end, remember every cloud has a silver lining. Medical diagnosis of the condition named Azoospermia itself runs chills down the spine and can make one feel hopeless and uncertain. This is the reality for many men facing azoospermia, a condition that impacts male fertility.
But with advancements in medical science, the condition is treatable therefore it is essential to understand the intricacies of azoospermia for every man. In this guide, we delve into the depths of azoospermia, unravel its causes, explore the available treatments, and empower men with the knowledge they need to navigate the path towards their fertility aspirations.
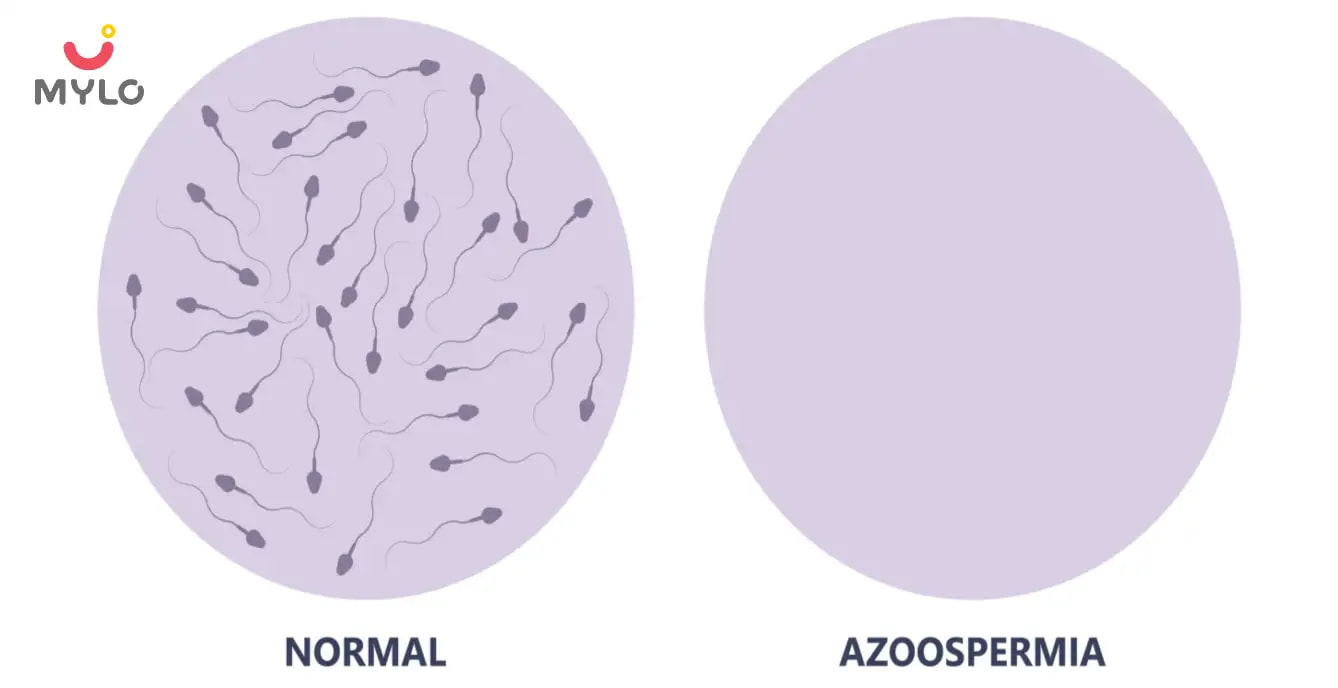
What is Azoospermia?
Azoospermia refers to a condition in which there is an absence of sperm in the semen. It is a significant concern for male fertility, as the absence of sperm can make it difficult or impossible for a man to father a child through natural conception. Understanding azoospermia is crucial for individuals and couples who are seeking to overcome fertility challenges and explore possible solutions.
What are the Types of Azoospermia?
Azoospermia can be categorized into two main types:
1. Obstructive Azoospermia
This type occurs when there is a blockage or obstruction in the male reproductive tract that prevents the sperm from being ejaculated. The testes continue to produce sperm, but it is unable to mix with semen due to the obstruction. Common causes of obstructive azoospermia include congenital abnormalities, previous infections, or vasectomy.
2. Non obstructive Azoospermia
In non obstructive azoospermia, there is a problem with sperm production in the testes. The testes either produce very few sperm or no sperm at all. This condition can be caused by genetic factors, hormonal imbalances, testicular injury, or certain medical treatments such as chemotherapy.
What are the Symptoms of Azoospermia?
Symptoms of Azoospermia include:
- Absence of sperm in semen
- Difficulty conceiving a child
- Normal sexual function and ejaculation
- No other apparent signs or symptoms
What Causes Azoospermia?
Azoospermia, the absence of sperm in the ejaculate, can be caused by various factors. These factors are dependent on the type of azoospermia. Some common causes of azoospermia are obstruction or blockage in the reproductive tract, hormonal imbalances, genetic disorders, and testicular injury or trauma. Other reasons are infections or inflammation, medications, and congenital conditions or birth defects.
Causes of Obstructive Azoospermia
Obstructive azoospermia occurs when there is a physical blockage or obstruction that prevents the sperm from reaching the semen. Some common causes of obstructive azoospermia include:
1. Vasectomy
Vasectomy is a surgical procedure in which the vas deferens, the tube that carries sperm from the testicles to the urethra, is cut and sealed. This intentional blockage prevents sperm from being ejaculated.
2. Congenital Anomalies
Some men are born with structural abnormalities in the reproductive tract that obstruct the passage of sperm. These anomalies can include absence or malformation of the vas deferens, epididymal cysts, or other congenital defects.
3. Infections and Inflammatory Conditions
Infections in the reproductive system, such as epididymitis or prostatitis, can cause inflammation and scarring that obstructs the sperm ducts. Sexually transmitted infections like chlamydia or gonorrhea can also lead to scarring and blockages.
4. Ejaculatory Duct Obstruction
The ejaculatory ducts are responsible for carrying sperm from the seminal vesicles to the urethra. Blockages or abnormalities in these ducts can prevent the sperm from being ejaculated. This condition can be congenital or acquired, and surgical intervention may be necessary to remove or bypass the obstruction.
5. Previous Surgeries or Trauma
Prior surgeries or trauma to the reproductive organs can result in scar tissue formation, which can lead to blockages. Procedures like hernia repairs, prostate surgeries, or testicular surgeries can inadvertently cause damage to the reproductive tract, leading to obstructive azoospermia.
Causes of Non Obstructive Azoospermia
Non obstructive azoospermia (NOA) is a condition characterized by the absence of sperm in the ejaculate due to problems with sperm production rather than blockages in the reproductive tract. Several factors can contribute to the development of non obstructive azoospermia, including:
1. Testicular Dysfunction
Testicular factors are the most common cause of NOA. These can include genetic abnormalities, such as Klinefelter syndrome or Y-chromosome microdeletions, which affect the proper development and function of the testes. Other conditions that can cause testicular dysfunction include testicular trauma, infections, radiation or chemotherapy treatment, and certain autoimmune disorders.
2. Hormonal Imbalances
Hormonal imbalances, particularly deficiencies in follicle-stimulating hormone (FSH) and luteinizing hormone (LH), can disrupt the production of sperm in the testes. Conditions such as hypogonadotropic hypogonadism and pituitary disorders can lead to hormonal imbalances and subsequently contribute to NOA.
3. Varicocele
Varicocele is a condition characterized by the enlargement of veins in the scrotum, which can lead to increased testicular temperature and impaired sperm production. It is a common and treatable cause of NOA.
4. Environmental Factors
Certain environmental factors can also play a role in the development of NOA. Exposure to chemicals, toxins, or radiation can have a detrimental effect on sperm production. Additionally, lifestyle factors such as excessive alcohol consumption, smoking, and drug abuse can contribute to reduced sperm production.
5. Idiopathic Causes
In some cases, the cause of NOA remains unknown, and it is referred to as idiopathic NOA. It is estimated that about 30% of cases fall under this category, where the specific cause cannot be identified.
You may like : Understanding Infertility: Causes, Symptoms, and Treatments
How is Azoospermia Diagnosed?
Azoospermia is typically diagnosed through a comprehensive evaluation that involves a series of tests and examinations. The diagnostic process for azoospermia includes:
1. Semen Analysis
The initial step is a semen analysis, which involves providing a semen sample for laboratory testing. The sample is examined under a microscope to assess the presence or absence of sperm.
2. Hormone Testing
Blood tests may be conducted to measure hormone levels, particularly follicle-stimulating hormone (FSH), luteinizing hormone (LH), testosterone, and prolactin.
3. Genetic Testing
Genetic testing may be recommended to identify any genetic abnormalities or chromosomal disorders that could be contributing to azoospermia. This testing is particularly important for men with non-obstructive azoospermia.
4. Physical Examination and Medical History
A comprehensive physical examination is performed to assess the reproductive organs and identify any abnormalities. A detailed medical history is also taken to evaluate factors such as past surgeries, infections, or exposure to toxins that may have contributed to azoospermia.
5. Imaging Tests
In some cases, imaging tests such as scrotal ultrasound or transrectal ultrasound may be performed to assess the structure of the reproductive organs and identify any abnormalities or obstructions.
You may like : Fertisure M: The Comprehensive Solution to Male Infertility and Reproductive Health
Azoospermia Treatment Options
Azoospermia treatment depend on the underlying cause and can vary from person to person. Here are some common treatment approaches:
1. Surgical Interventions
Surgical procedures may be recommended for obstructive azoospermia to address any blockages or obstructions in the reproductive tract. These procedures can include vasectomy reversal, epididymal or testicular sperm extraction (TESE), or vasoepididymostomy.
2. Hormone Therapy
Hormone therapy may be beneficial for men with hormonal imbalances that contribute to azoospermia. This involves the administration of specific hormones, such as follicle-stimulating hormone (FSH), to stimulate sperm production in the testes.
3. Assisted Reproductive Techniques
In cases of non-obstructive azoospermia or when surgical interventions are not possible or successful, assisted reproductive techniques can be utilized. These techniques include in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI).
4. Donor Sperm
In cases where it is not possible to retrieve sperm or if the male partner has a genetic condition that could be passed on to offspring, the use of donor sperm can be an option. Donor sperm can be used in intrauterine insemination (IUI) or IVF procedures to achieve pregnancy.
Final Thoughts
In conclusion, azoospermia is a condition that affects male fertility and refers to the absence of sperm in the ejaculate. Fortunately, there are treatment options available, ranging from surgical interventions to assisted reproductive techniques. It's essential for men facing azoospermia to seek medical guidance and explore the available options to address the condition and fulfill their desire for parenthood.
References
1. Jarvi, K., Lo, K., Grober, E., Mak, V., Fischer, A., Grantmyre, J., Zini, A., Chan, P., Patry, G., Chow, V., & Domes, T. (2015). The workup and management of azoospermic males. Canadian Urological Association Journal, 9(7-8), 229–235.
2. Sharma, M., & Leslie, S. W. (2022). Azoospermia. PubMed; StatPearls Publishing.



Written by
Madhavi Gupta
Dr. Madhavi Gupta is an accomplished Ayurvedic doctor specializing in Medical content writing with an experience of over 10 years.
Read MoreGet baby's diet chart, and growth tips
Related Articles
Related Topics
RECENTLY PUBLISHED ARTICLES
our most recent articles

Infertility
Premature Ovarian Failure: How it Affects Female Fertility and What You Can Do About It

Male Infertility
Erectile Dysfunction: What Causes It and How to Treat It
In Vitro Fertilization (IVF)
Positive Signs After Embryo Transfer: What to Look Out For
IVF Pregnancy
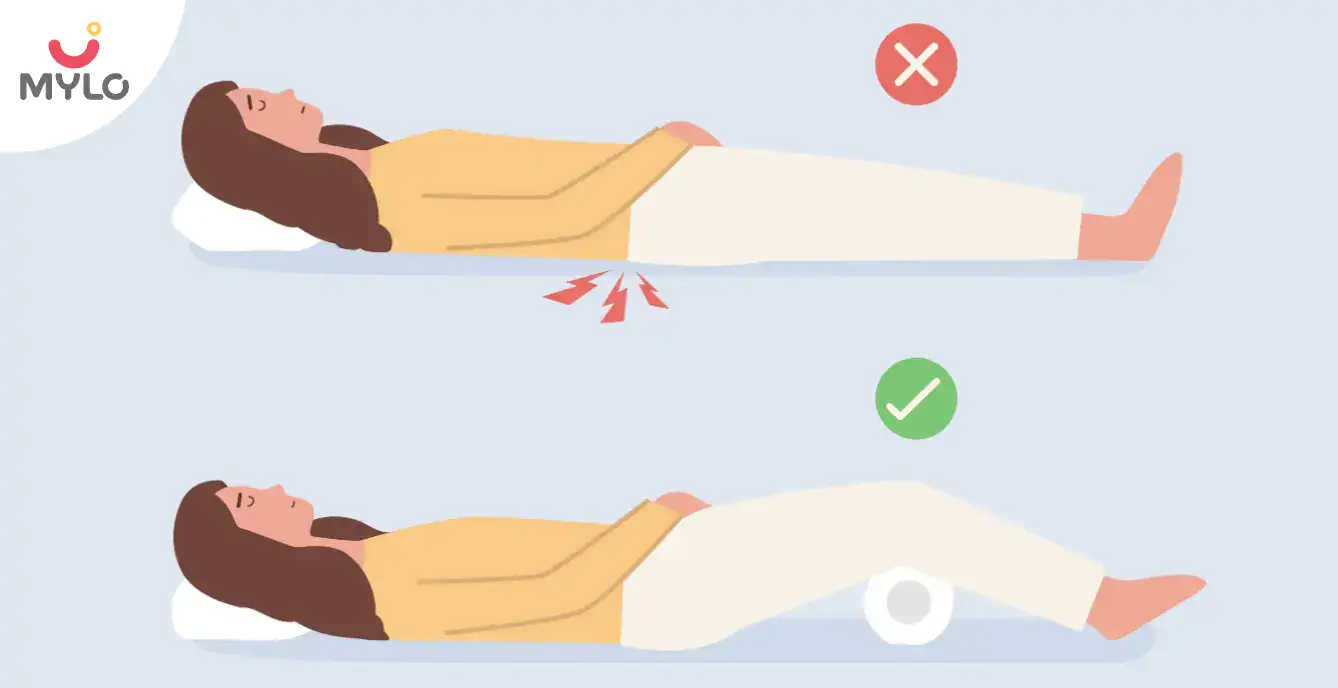
Sleeping Position After IVF & Other Precautions That Can Boost Your Chances of Success

IVF Pregnancy
IVF Failure Reasons: Exploring the Challenges Couples Face with Infertility

Ayurveda & Homeopathy
Putrajeevak Beej: The Ancient Seed for Modern Health and Fertility
- Shivlingi Beej: The Ultimate Guide to Boosting Your Fertility Naturally
- Milk Thistle in Ayurveda: Unlock The Healing Potential and Health Benefits of This Herb
- Orchidopexy: All You Need to Know About Its Procedure, Risks, and Recovery
- Transvaginal Ultrasound: A Non-Invasive Tool for Early Detection of Reproductive Health Issues
- New Mom Diet Plan – Month 11 Week 42
- Ejaculatory Duct Obstruction: How It Affects Male Fertility and What You Can Do About It
- Testicular Ultrasound: What You Need to Know About the Procedure and Its Benefits
- Symptoms of Low AMH to Watch Out For: A Health Alert for Women Trying to Conceive
- Hysteroscopy: Everything You Need to Know About This Minimally Invasive Procedure
- Dalchini: How This Herb Can Make Way From Your Spice Rack to Your Medicine Cabinet
- Fenugreek Powder: Health Benefits of Fenugreek From Your Kitchen to Your Medicine Cabinet
- Moringa Powder: The Superfood You Need in Your Diet for a Healthy Lifestyle
- Genital Herpes: Causes, Symptoms, Risks & Treatment
- Ashokarishta: All You Need to Know About This Miracle Tonic for Women


AWARDS AND RECOGNITION

Mylo wins Forbes D2C Disruptor award

Mylo wins The Economic Times Promising Brands 2022
AS SEEN IN
















- Mylo Care: Effective and science-backed personal care and wellness solutions for a joyful you.
- Mylo Baby: Science-backed, gentle and effective personal care & hygiene range for your little one.
- Mylo Community: Trusted and empathetic community of 10mn+ parents and experts.
Product Categories
baby carrier | baby soap | baby wipes | stretch marks cream | baby cream | baby shampoo | baby massage oil | baby hair oil | stretch marks oil | baby body wash | baby powder | baby lotion | diaper rash cream | newborn diapers | teether | baby kajal | baby diapers | cloth diapers |