Home

In Vitro Fertilization (IVF)

Types of IVF, Their Benefits and Side Effects Everything You Need to Know..
In this Article
In Vitro Fertilization (IVF)
Types of IVF, Their Benefits and Side Effects Everything You Need to Know..
Updated on 16 August 2023
IVF, or In Vitro Fertilization, is a widely used assisted reproductive technology that helps individuals and couples struggling with infertility to conceive. There are several types of IVF treatment available, each with its own unique benefits and possible side effects. In this comprehensive guide, we will explore the different types of IVF, discuss their advantages and disadvantages, and shed light on the potential side effects associated with each procedure.
Types of IVF
In vitro fertilization (IVF) procedures that can be used depending on the specific needs and circumstances of the individual or couple. Let’s discuss the different types of In-Vitro Fertilization procedures available:
1. Natural IVF
Natural IVF is a procedure that closely mimics a woman's natural menstrual cycle. It involves collecting the egg that is naturally produced during the cycle, without the use of fertility drugs to stimulate multiple egg production. This approach is suitable for women who do not respond well to fertility medications or prefer a more natural approach to IVF.
One of the main benefits of natural IVF is the reduced risk of ovarian hyperstimulation syndrome (OHSS), a potentially serious condition that can occur when the ovaries are overstimulated. However, since only one egg is typically retrieved during natural IVF, the success rates may be lower compared to other types of IVF treatment.
2. Mini IVF (minimal stimulation)
Mini IVF, also known as minimal stimulation IVF, is a variation of traditional IVF that uses lower doses of fertility medications to stimulate the ovaries. The aim is to retrieve a smaller number of high-quality eggs, rather than a larger quantity of eggs. This approach is often recommended for women who are at a higher risk of ovarian hyperstimulation syndrome or have a low ovarian reserve.
One of the main advantages of mini IVF is the reduced cost associated with lower medication doses. Additionally, the milder stimulation can lead to a more comfortable experience for the patient. However, since fewer eggs are retrieved, the chances of successful fertilization and implantation may be lower.
3. IVF with Elective Single Embryo Transfer (eSET)
IVF with Elective Single Embryo Transfer, or eSET, is a procedure where only one embryo is transferred to the uterus, even if multiple embryos are available. This approach is aimed at reducing the risk of multiple pregnancies, which can pose health risks to both the mother and the babies.
The main benefit of eSET is the decreased likelihood of multiple pregnancies, which can lead to complications such as preterm birth and low birth weight. By transferring a single embryo, the chances of a successful pregnancy are slightly lower compared to transferring multiple embryos. However, advancements in embryo selection and screening techniques have significantly improved the success rates of eSET.
4. IVF with Intracytoplasmic Sperm Injection (ICSI)
IVF with Intracytoplasmic Sperm Injection, or ICSI, is a specialized form of IVF that involves the direct injection of a single sperm into each mature egg. This technique is typically used when there are issues with sperm quality, such as low sperm count or poor sperm motility.
The main benefit of ICSI is the ability to overcome male infertility factors by directly injecting a healthy sperm into the egg. This significantly increases the chances of successful fertilization and embryo development. However, there is a slightly higher risk of genetic abnormalities associated with ICSI, as the natural selection process of sperm is bypassed.
5. IVF with Frozen Embryo Transfer (FET)
IVF with Frozen Embryo Transfer, or FET, involves the freezing and storage of embryos from a previous IVF cycle, which are then thawed and transferred to the uterus at a later time. This approach allows for more flexibility in timing and can increase the chances of a successful pregnancy.
One of the main benefits of FET is the ability to optimize the timing of embryo transfer, as it allows for better synchronization between the embryo and the uterine lining. Additionally, frozen embryos have been shown to have comparable pregnancy rates to fresh embryos. However, the process of freezing and thawing embryos can decrease the overall success rates of IVF.
6. IVF with Egg Donor
IVF with an egg donor is a type of in vitro fertilization (IVF) procedure where the eggs used for fertilization come from a donor instead of the intended mother. This procedure is typically recommended for women who are unable to produce viable eggs or have a high risk of passing on genetic disorders.
The process involves selecting a suitable egg donor who undergoes ovarian stimulation to produce multiple eggs. The eggs are then retrieved and fertilized with the partner's or donor's sperm in the laboratory. The resulting embryos are cultured and assessed for quality before being transferred into the uterus of the intended mother or a gestational carrier for implantation.
7. IVF with Donor Sperm
IVF with donor sperm is a procedure where the sperm used for fertilization comes from a donor instead of the male partner of the intended mother. This treatment option is suitable for couples with severe male infertility.
The process begins with the selection of a sperm donor, who can be anonymous or known. The donor's sperm undergoes rigorous testing for communicable diseases before being made available for use. The IVF process with donor sperm is similar to a regular IVF cycle, involving medication to stimulate egg production, egg retrieval, fertilization in the laboratory, and embryo transfer. This procedure offers hope and a pathway to parenthood for individuals facing barriers to conception.
You may also like : TESA IVF: How This Procedure Can Help You Achieve Your Dream of Parenthood
Let us now understand the advantages and disadvantages of IVF.
What are the Benefits of IVF?
Here are some common advantages of IVF:
1. Increased chances of pregnancy
IVF offers hope to individuals and couples who have been struggling to conceive naturally. By bypassing certain fertility barriers, IVF can significantly increase the chances of achieving a successful pregnancy.
2. Genetic screening
IVF procedures often involve the option for genetic screening of embryos before implantation. This allows for the identification of any genetic abnormalities, reducing the risk of passing on inheritable diseases to the child.
3. Option for single embryo transfer
With advancements in IVF techniques, it is now possible to transfer a single embryo, reducing the risk of multiple pregnancies and associated complications.
4. Use of donor eggs or sperm
IVF provides the option to use donor eggs or sperm, allowing individuals and couples with certain fertility issues to still experience pregnancy and childbirth.
5. Psychological support
IVF clinics often provide counseling and support services to help individuals and couples navigate the emotional and psychological challenges associated with infertility and the IVF process.
You may also like : Difference Between IUI and IVF: Which is Better for You?
What are the Side Effects of IVF Treatment?
Let us now take a look at some common IVF side effects that one may experience during or after the treatment:
1. Ovarian hyperstimulation syndrome (OHSS)
This is a potential side effect of IVF treatment that occurs when the ovaries become overstimulated by fertility medications. Symptoms can range from mild discomfort to severe abdominal pain and fluid accumulation in the chest and abdomen.
2. Multiple pregnancies
One of the risks associated with IVF is the possibility of multiple pregnancies, which can increase the likelihood of complications such as premature birth and low birth weight.
3. Emotional and psychological effects
The emotional and psychological toll of IVF treatment can be significant. The stress of the process, along with the uncertainty of the outcome, can lead to feelings of anxiety, depression, and frustration.
4. Financial burden
IVF treatment can be costly, and the financial burden can add additional stress to individuals and couples undergoing the procedure. Insurance coverage for IVF varies widely, and many people have to bear the expenses out of pocket.
FAQs
1. What are the three types of IVF?
The three types commonly practiced are Natural IVF, Mini IVF, and IVF with Elective Single Embryo Transfer (eSET). Each type of IVF has its own unique benefits and considerations, and the choice depends on the specific circumstances and preferences of the individual or couple undergoing the procedure.
2. Which IVF cycle is most successful?
The success of an IVF cycle depends on various factors, including the age of the woman, the quality of the embryos, and the underlying cause of infertility. Generally, IVF with eSET has shown promising success rates, as it allows for the transfer of a single high-quality embryo, reducing the risk of multiple pregnancies.
3. Does IVF have a 100% success rate?
Despite the advancements in IVF technology, it is important to note that IVF does not guarantee a 100% success rate. Success rates vary depending on individual circumstances, and factors such as age, underlying fertility issues, and overall health can influence the outcome of the procedure.
Final Thoughts
IVF is a remarkable medical advancement that has helped millions of individuals and couples achieve their dream of having a child. By understanding the different types of IVF, their benefits, and possible side effects, individuals can make informed decisions about their fertility treatment options. It is important to consult with a fertility specialist who can provide personalized guidance and support throughout the IVF journey. Remember, each person's fertility journey is unique, and there is no one-size-fits-all approach. With the right medical care and emotional support, IVF can offer hope and the possibility of starting or expanding a family.
References
1. Wang J, Sauer MV. (2006). In vitro fertilization (IVF): a review of 3 decades of clinical innovation and technological advancement. Ther Clin Risk Manag.
2. Eftekhar M, Mohammadian F, Yousefnejad F, Molaei B, Aflatoonian A. (2012). Comparison of conventional IVF versus ICSI in non-male factor, normoresponder patients. Iran J Reprod Med.



Written by
Anupama Chadha
Anupama Chadha, born and raised in Delhi is a content writer who has written extensively for industries such as HR, Healthcare, Finance, Retail and Tech.
Read MoreGet baby's diet chart, and growth tips
Related Articles
Related Questions
Hello frnds..still no pain...doctor said head fix nhi hua hai..bt vagina me pain hai aur back pain bhi... anyone having same issues??

Kon kon c chije aisi hai jo pregnancy mei gas acidity jalan karti hain... Koi btayega plz bcz mujhe aksar khane ke baad hi samagh aata hai ki is chij se gas acidity jalan ho gyi hai. Please share your knowledge

I am 13 week pregnancy. Anyone having Storione-xt tablet. It better to have morning or night ???

Hlo to be moms....i hv a query...in my 9.5 wk i feel body joint pain like in ankle, knee, wrist, shoulder, toes....pain intensity is high...i cnt sleep....what should i do pls help....cn i cosult my doc.

Influenza and boostrix injection kisiko laga hai kya 8 month pregnancy me and q lagta hai ye plz reply me

RECENTLY PUBLISHED ARTICLES
our most recent articles

Feeding from a Bottle
How to Sterilize Baby Bottles: The Ultimate Step-by-Step Tutorial

Diet & Nutrition
What to eat when trying to conceive

White Discharge
White Discharge After IUI: Is It Normal & When to See a Doctor

Diet & Exercises Your Wife Can Follow During Pregnancy

Can a diet plan help deal with infertility in women and boost the chances of conception?
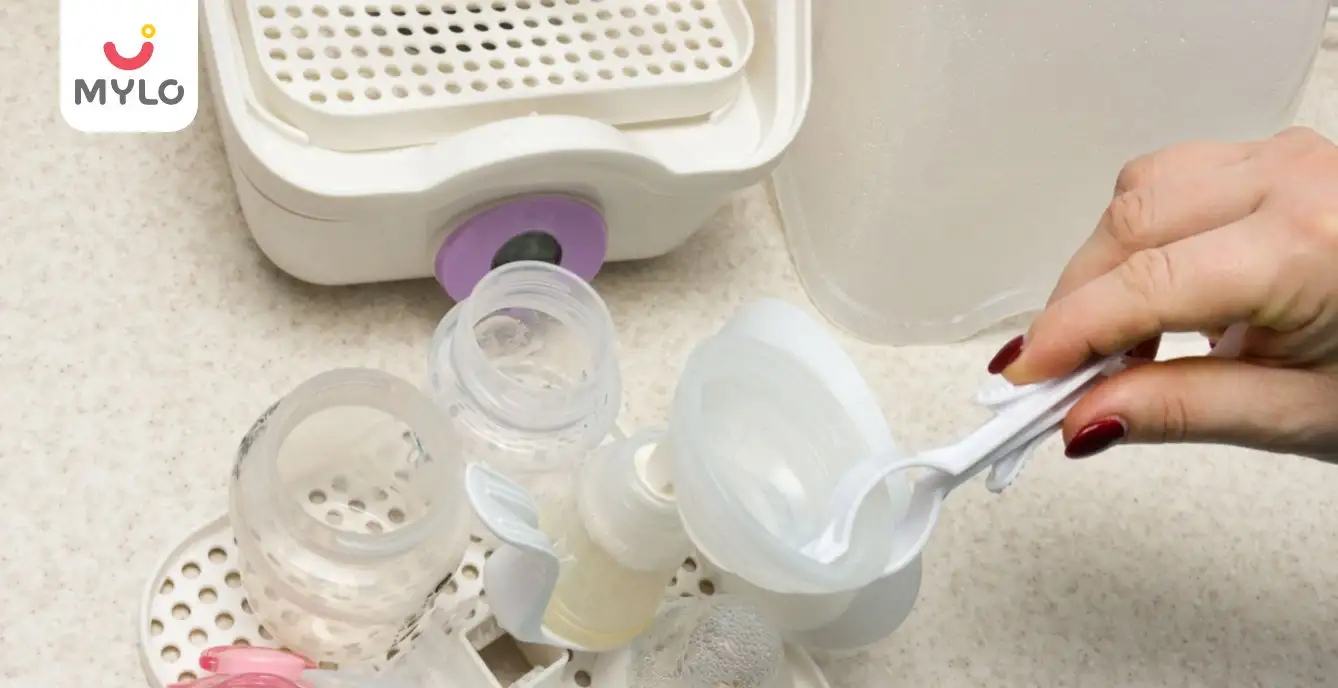
Pumping
How to Sterilize Breast Pump: A Comprehensive Guide for New Moms
- Bronchiectasis Meaning in Hindi | ब्रोन्किइक्टेसिस क्या होता है?
- The Ultimate Guide to Teej 2023: Celebrations, Traditions, and Dates
- Should I Pee After Sex if Trying to Get Pregnant? And 5 Other FAQs
- Menorrhagia: A Guide to Understanding Heavy Period Bleeding (Part 1)
- Indigestion and Heartburn During Pregnancy
- Understanding Follicular Study: A Comprehensive Guide to Female Fertility
- Maternity Fashion: How to Dress in Style in Each Trimester of Your Pregnancy?
- Oligomenorrhea: What Every Woman Needs to Know About Irregular Periods
- Can a Woman with Thyroid Problems Get Pregnant: Conceiving Against the Odds
- Adenomyosis Vs Endometriosis: How to Spot the Symptoms and Seek Early Intervention
- Fertility Test for Men and Women: What to Expect and Next Steps
- Reason for Irregular Periods After Marriage: A Comprehensive Guide
- How Soon Can You Get Pregnant After Stopping the Pill?
- Watery Semen: Is It Normal or a Sign of an Underlying Condition?


AWARDS AND RECOGNITION

Mylo wins Forbes D2C Disruptor award

Mylo wins The Economic Times Promising Brands 2022
AS SEEN IN
















- Mylo Care: Effective and science-backed personal care and wellness solutions for a joyful you.
- Mylo Baby: Science-backed, gentle and effective personal care & hygiene range for your little one.
- Mylo Community: Trusted and empathetic community of 10mn+ parents and experts.
Product Categories
baby carrier | baby soap | baby wipes | stretch marks cream | baby cream | baby shampoo | baby massage oil | baby hair oil | stretch marks oil | baby body wash | baby powder | baby lotion | diaper rash cream | newborn diapers | teether | baby kajal | baby diapers | cloth diapers |